2025 International Fall Summit
October 15, 2025 | 12:00 PM EST
COST AVOIDANCE & WASTE TRACKER
Too often, a medication is prescribed, processed, and filled but not used by the patient. In cases like these, patients, pharmacies, and practices all lose out. The Cost Avoidance and Waste Tracker (CAWT) helps identify and prevent drug waste by facilitating interventions at the practice level.


HOW IT WORKS
NCODA’s proprietary CAWT tool measures cost avoidance within an MID versus the waste produced by specialty and mail-order pharmacies. Just input your practice’s data and this simple web tool calculates your cost and waste numbers in a simple visual format. Because it’s easy to use and simplifies sharing individual and compiled data, it helps make a case for the Medically Integrated Dispensary.
Benefits of the Cost Avoidance and Waste Tracker Tool
The tool defines waste as drugs that have been processed or prescriptions filled, and then, for any reason, the patient does not use the drug. Cost avoidance is any intervention made before the drug is dispensed that prevents waste. Using NCODA’s Cost Avoidance and Waste Tracker tool, you’ll be able to quantify both the costs of waste and the benefits of cost avoidance at your practice using your data. This is helpful for:
- Demonstrating the benefits of MID to third-party payers
- Providing CAWT data for insurance input
- Quantifying the benefits of MID institutions
- Quantify Your Practice Data. Become a Member.
Already a member? Login to use this tool.
Making the Case for Medically Integrated Dispensing and Better Patient Care
The Cost Avoidance and Waste Tracker tool shows the significant impact that MIDs can have on cost avoidance interventions when compared to the waste produced through other forms of oncology distribution. Using this tool to compile your data, you can help uncover the financial influence and positive change that MIDs bring to the oncology marketplace.
Read more from the Journal of Oncology →Frequently Asked Questions
The Cost Avoidance and Waste Tracker (CAWT) is a tool developed by NCODA to help healthcare practices identify and prevent medication waste by facilitating interventions at the practice level.
- “Cost Avoidance” interventions often occur before a medication being is dispensed to the patient that preclude an unnecessary prescription from being filled and sent to the patient. These interventions allow the patient to maximize their medication.
- Examples:
- A patient’s therapy was held for a week so the dispensing pharmacy short fills the next prescription so that the medication that was held can still be used.
- A patient’s disease progresses, the doctor decides to switch medications, and the medically integrated pharmacy sees the patients’ chart note and contacts the dispensing pharmacy before the medication is refilled.
- “Waste” is when a medication is filled and dispensed to a patient that, for any reason, is not used. This can either be a partial or full supply of a medication.
- Examples:
- A patient experiences adverse event(s) on the medication near the end of a cycle, so they contact their provider. The provider makes the decision to hold the medication. The mail order pharmacy has already sent the prescription so that the patient has it in time to start the next cycle. The provider then makes the decision to discontinue the medication leading to a medication waste.
- A patient goes on hospice and decides to stop their treatment(s). Any medication(s) not used that were previously dispensed becomes waste.
- When inputting data into the CAWT, the required fields are:
- The date the medication was received/intervention occurred
- The type of insurance
- Payer
- Dispensing pharmacy
- Medication name
- Medication strength
- How many tablets/capsules were avoided/wasted
- Whether it was considered a “cost avoidance” or “waste”
- Whether the medication was a full fill or a partial fill
- The other fields (“date medication was dispensed,” “BIN,” “PCN,” “PBM,” “PBM Group,” “Reasons”) are all optional. Many practices use these fields to pinpoint where data is coming from. This allows practices to have individualized conversations with payers.
- When you login to use the CAWT tool, your practice information from your profile will pull across and will autofill in for that section.
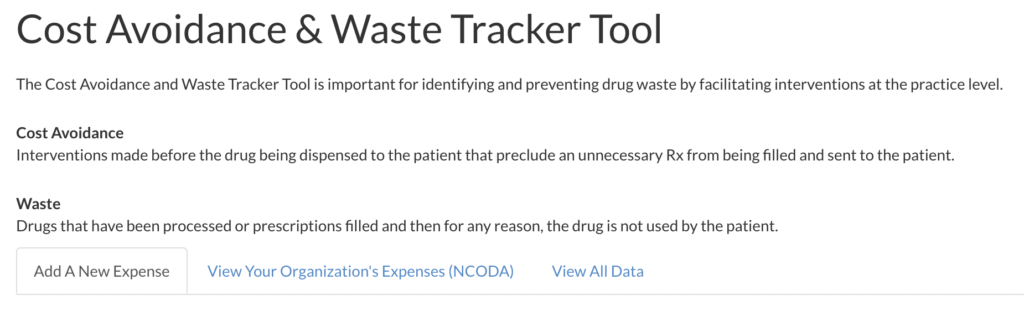
- There will be a tab called “View Your Organization’s Expenses” as seen above.
- When you click on this tab it will allow you to see the data that has been input from your practice.
- Individual practice data is hidden and not shared across membership.
- The pricing is updated on a quarterly basis and uses average wholesale cost (AWC) for the standard.
- All pricing comes from Red Book and does not reflect individual contracting or rebates.
- Total expense calculated is from a unit perspective, and it provides a ‘per pill’ cost.
- Practices can use the information when having contracting discussions with payers, as well as when advocating for the value of their medically integrated practice.
- Tracking interventions allows for an overall idea of additional costs or savings that are happening in your practice.
- NCODA does not share any individual practice data with outside sources.
- NCODA does report on the aggregate information to advocate for better patient care.
- Most cancer medications supplied through specialty pharmacy distribution are included.
- Medications and strengths are updated during quarterly reviews.
- When selecting the “type” you can select “Patient Assistance Programs” and then include the program information in the payer field.
- Date Medication Received/Intervention: When the medication was provided to the patient, or the intervention took place. If a patient is relying on a mail-order pharmacy, it would be when the patient receives the medication. If it is an intervention for a cost avoidance a patient would not be receiving so you track the day the intervention occurred.
- Date Medication Dispensed: When the medication was dispensed to the patient. This can be the date it was sent out by a mail-order pharmacy or the day the prescription was filled.
- This field is where we track the type of insurance or assistance the patient is using to cover the prescription. Examples include Medicare, Medicaid, private insurance, patient assistance programs, or co-pay cards.
- The dispensing pharmacy is where the medication is being dispensed from. You have a few options here; you can either select your own practice, in-house dispensing pharmacy, or you can select the outside mail-order pharmacy that the prescription is coming from.
- The BIN, or bank identification number, is part of your insurance.
- This is a six-digit number attached to where the health insurance provider is to receive the claim for your prescription. This is how the claim is sent for billing.
- Also referred to as a “group number” (RxGrp), this is a code that allows the PBM to track the specific employer’s insurance plan.
- Each employer chooses a package for their employees based on price or types of coverage. This is identified through the group number.
- PCN stands for “processor control number.”
- Just like the BIN and PBM Group, the PCN is an additional identifier used by insurance companies to determine which processor will handle your claim.
- The PCN is also connected to the patient’s prescription drug plan.
- Medically integrated dispensing refers to your own practice’s pharmacy. You have the option of either selecting your practice or using this option.
- Since your practice information is already attached with the data, this is an easier way of saying you dispensed the medication.
- No.
- Many practices find that it is easier to set aside time to input information all at once.
- Practices make note of “waste” or “cost avoidance” throughout the week and then when there is a break in workflow, they enter them all in at once.
- If you find yourself in a career change and are not at another practice, all you have to do is make sure that your NCODA “member profile” is updated with the new practice information, including your new email address.
- Once updated, you will automatically be switched over to the new practice site.
- Please reach out to Austin Starkey (austin.starkey@ncoda.org) for any questions or comments. If you would like to schedule a walkthrough of the tool please select your availability here.